We're tearing down barriers
To

birth control
Trust Her provides access to all forms of contraception.
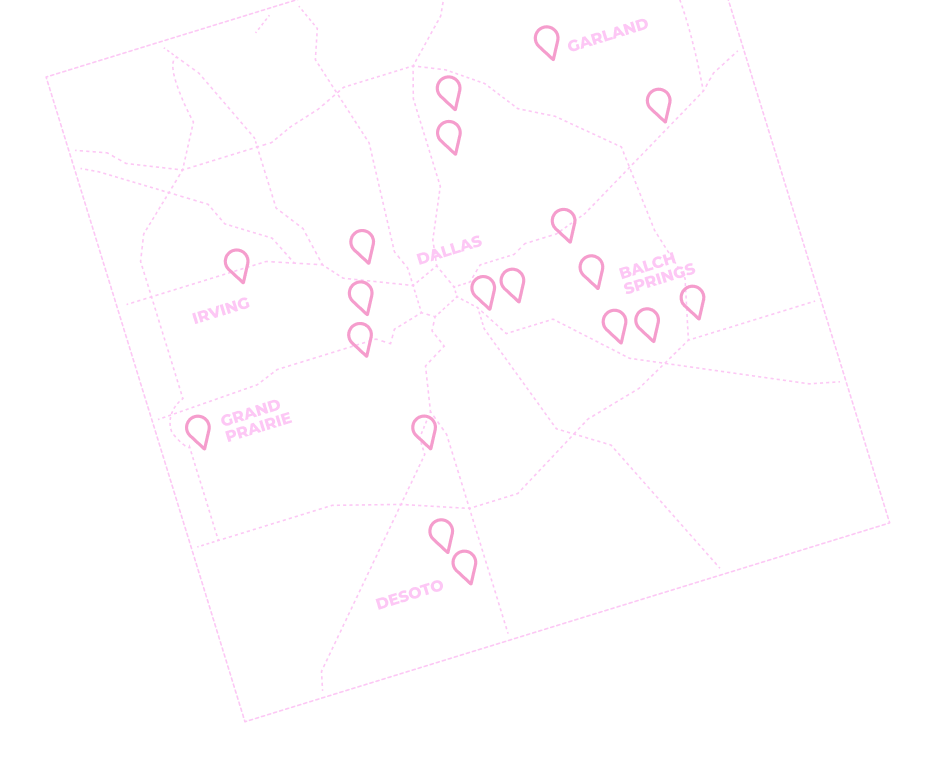
How can I get free birth control in Dallas?
Visit a Trust Her Access Clinic, where providers can help you:
- Enroll in programs like Medicaid and Healthy Texas Women that cover 100% of the cost of birth control.
- Receive a sliding fee discount, where you pay a lower cost for care based on your income.
- Get free birth control from Trust Her, if you’re eligible.
am I eligible?

Learn more about birth control and sexual health
Find out more about different birth control methods, and check out our guides for teens and parents!
Women report that contraception helps them achieve their goals for education, financial stability, career growth, and family success.
Join the movement in Dallas.

Today, 1.8 million Texas women of childbearing age cannot afford birth control.
It can take a Texas woman 7 months or more to obtain her contraceptive of choice.

Low-income women of color are more likely to report challenges obtaining their birth control method of choice.